In the United States, ticks can carry pathogens that cause diseases in humans, such as Lyme disease, Babesia, Bartonella, Colorado tick fever, Heartland virus, and Rocky Mountain Spotted Fever. While it used to be more prominent in the Northeast, Lyme disease is now present in all 50 states and is the most common tick-borne disease in the United States. If left untreated, Lyme Disease and other tick-borne illnesses can wreak havoc on human health.
One of the earliest signs of Lyme Disease is the characteristic red rash that can appear within a few weeks of a tick bite. Initially, the bite looks like a small red spot at the bite site; over time, the spot expands and forms a circle that often resembles a bullseye and can vary greatly in size. While this rash is pathognomonic of Lyme, it is only seen in 20-40% of patients. Early symptoms can also mimic the flu and include fever, headache, stiff neck, body aches, and fatigue. About 60% of people who are not treated early with antibiotics develop recurring attacks of arthritis that last anywhere from a few days to a few months, most commonly in the knees. Neurological and heart problems can also appear several weeks or even years after the initial tick bite if the infection goes untreated. Stiff neck and severe headache that indicate meningitis, temporary paralysis of muscles in the face resembling Bell’s palsy, numbness, pain or weakness in the limbs, and poor motor coordination may also occur. In addition, some people have reported heart abnormalities such as palpitations, lightheadedness, fainting, chest pain, and shortness of breath, although these symptoms are less common.
The good news is that many people with Lyme disease are treated successfully with antibiotics and recover completely. Still, some people don’t have the typical symptoms, and some don’t fully recover after antibiotics. These patients can develop a Chronic Persistent Lyme syndrome that includes a wide variety of symptoms that can mimic many other diseases, including autoimmune diseases like Lupus and Rheumatoid Arthritis, neurologic illnesses such as Parkinson’s Disease and dementia, and Chronic Fatigue Syndrome.
Some people are more likely to struggle with this Chronic Lyme syndrome than others. This is partly due to genetics, as some people’s immune systems are less likely to recognize and eliminate the bacteria. Another issue is that some people are better at eliminating inflammation and toxins from their system. People with more efficient liver enzymes and less inflammation are less likely to feel sick. We help people minimize toxins going in and enhance detoxification to decrease symptoms and aid in healing.
In addition, the ticks that carry Lyme disease often carry other bacteria and parasites, such as Bartonella and Babesia. These agents, known as co-infections, also cause several significant symptoms (see below). Like Lyme, these co-infections can also interfere with the immune system, thus keeping themselves and the Lyme in the body longer and increasing the inflammatory level in the bucket. Patients with Chronic Lyme disease also commonly have other toxins in their system, such as mold toxins, heavy metals, and parasites. This further complicates the clinical picture, and the treatment of Lyme necessarily involves the removal of these other toxins. This can make the treatment process long and complicated.

CO-INFECTIONS:
Babesiosis: Symptoms are similar to Lyme disease, but this illness often starts with a high fever and chills. As the infection develops, patients may notice fatigue, pounding headaches, drenching sweats, muscle aches, chest pain, hip pain, and shortness of breath. Babesiosis is often very mild, but regardless of symptom severity, can be life-threatening to the elderly, and those with compromised immune systems.
Bartonella: Early signs include fever, fatigue, headache, poor appetite, and an unusual streaky rash resembling stretch marks; swollen glands around the head, neck, and arms are also common. Patients with Bartonellosis are more likely to have neurological symptoms such as blurred vision, numbness or burning of the extremities, memory loss, balance problems, photosensitivity, headaches, ataxia, and tremors. Psychiatric manifestations can also occur, but are more rare.
Rickettsia: Bacteria include both the spotted fever group, and the typhus group. Rocky Mountain Spotted Fever is the most common type in the US, and can range from mild illness to fatal illness. Initial symptoms are high fever, severe headache, abdominal pain, and muscle pain. A spotted rash beginning at the wrist or ankles is typical.
Ehrlichiosis and Anaplasmosis: Characterized by sudden high fever, fatigue, muscle aches, and headache. Severity ranges from mild to life-threatening. Those who are severely ill can have low white blood cell count, low platelet count, anemia, elevated liver enzymes, kidney failure, and respiratory insufficiency. Anyone with a suppressed immune system is more likely to suffer from a severe case.
Besides these common co-infections, there are others which vary based upon the geographical location of the tick. Colorado tick fever virus, mycoplasmas, Powassan encephalitis virus, other forms of Borrelia, and tularemia can occur and are characterized by symptoms similar to those mentioned above.
There is also a connection between chronic Lyme disease and mold illness:
There is research that shows up to one half of all unresolved Lyme disease cases are due in part to the inflammation that is caused by mold illness: exposure to both mold and Lyme are very common, and their symptoms often overlap. Both mold illness and Lyme disease symptoms are caused by immune system dysregulation and the overproduction of pro-inflammatory proteins in the body.
When an individual is dealing with Lyme disease and has also been exposed to mold, their bodies and immune system can weaken significantly. The same is true if an individual is suffering from mold illness and is then exposed to Lyme. Unfortunately, having one of these conditions makes individuals more susceptible to the other, and here at AIM, we see many patients dealing with both.
PREVENTION:
Those who live near heavily wooded areas, or those who spend a lot of time in these areas, are at increased risk of being bitten by a tick carrying a dangerous pathogen. Infection is more likely to occur during the summer and the fall, although numbers have increased during the springtime in recent years. Ticks are most active between the months of April-September.
Fortunately, there are many ways to prevent Lyme disease and to prevent tick bites altogether. The first step in prevention is knowing where to expect ticks. Ticks live in grassy, brushy, or wooded areas and on animals. Deer are known to carry the ticks that cause Lyme disease. Spending time outside walking your dog, doing yard work, camping, gardening, or hunting can put you at risk of encountering ticks.
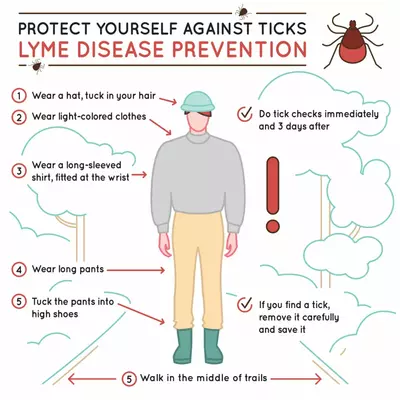
Be sure to walk in the center of trails when hiking and check your clothing and your gear for ticks before going inside. Tucking pants into socks can also offer protection. Tumble drying clothes in the dryer on high heat for 10 minutes will kill ticks on dry clothing.
For added protection against ticks, consider using a natural repellant. Using essential oils can be a safe, non-toxic alternative to insect repellants containing chemical ingredients that can be harmful to human health. An essential oil blend including Citronella, lemongrass, rosemary, geranium, spearmint, thyme, and clove has been tested and been shown to repel ticks, as well as mosquitoes and fleas. Visit our Lifestyle Store or give us a call to purchase this essential oil blend.
The chemical repellant options which are most effective, but also more toxic, include DEET and Picardin. The best way to use these is to put them on clothing (hat brims, neck and cuffs of shirts, and bottom of pants and boots). If you put these on the skin, always wash them off after your hike. Do not use these on young children without discussing them first with your child’s doctor.
BOTTOM LINE:
Here at AIM, we work with labs that specialize in finding tick-borne pathogens, and mold, and other toxins in your system, so we can get to the root cause of your illness and treat you effectively.
Treatment duration for Lyme disease and mold toxin illness can vary greatly. Traditional antibiotic treatment for Acute Lyme disease is 2-4 weeks, but patients with Chronic Persistent Lyme require longer treatment periods and more complex interventions depending on the extent of the disease and the presence or absence of other toxins and co-infections.
If you believe you have come into contact with a tick or have been exposed to mold, and you are suffering from any of the symptoms mentioned above, it’s very important to consult with your physician so that the appropriate testing and treatment can be ordered.









